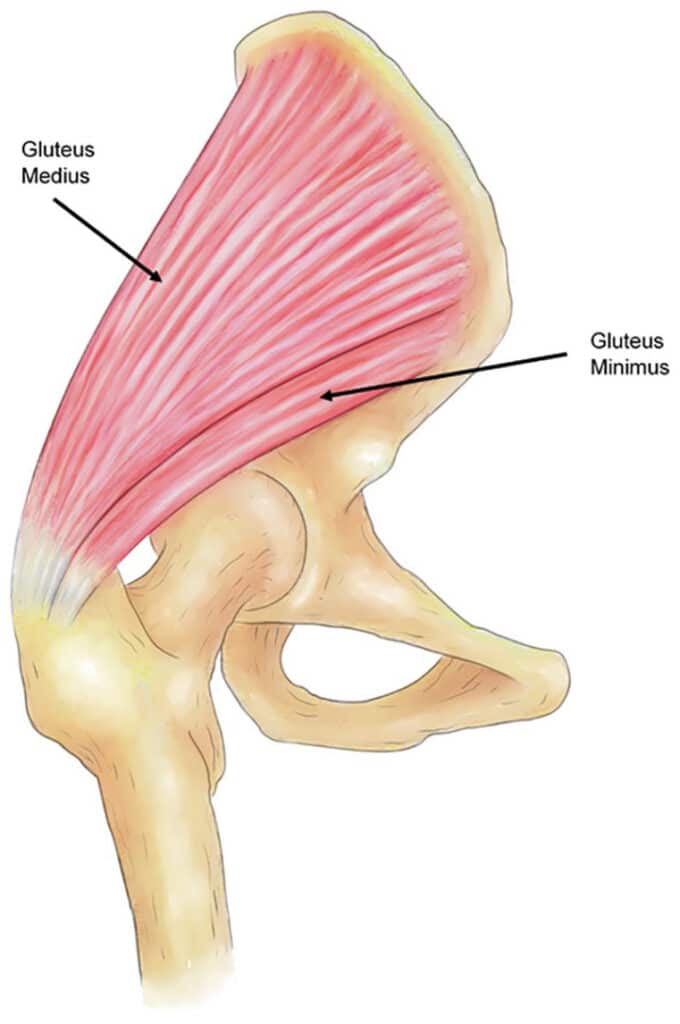
Pain over the outside of the upper thigh bone (femur) may be caused by problems with the gluteal tendons. There are 3 gluteal muscles around the hip – the Gluteus Maximus which forms the buttock is the largest and sits behind the hip joint and femur. The two smaller muscles, Gluteus Medius and Gluteus Minimus lie underneath this and join the side of the pelvic bone (ilium) to the top of the femur. They are attached to the outside of the upper femur (the greater trochanter) by strong tendons and act to lift the leg out to the side, a movement known as abduction. Gluteal tendons are often referred to as “abductor” tendons as a result. During normal walking, these muscles stabilise the hip and keep the pelvis level when the opposite foot comes off the ground. This requires them to transmit large forces, typically 2-3 times body weight and over time this may lead to tendon wear.
Lying over the tendons is a small piece of tissue known as the trochanteric bursa – this contains a small amount of fluid and acts to minimise friction from the tough layer of connective tissue (known as the iliotibial band or ITB) that runs over the outside of the femur, down the outside of the leg all the way to the upper shin bone (tibia). Inflammation of this bursa, or a tight ITB can also cause pain and hence these symptoms may also be described as “Trochanteric Bursitis” or “Greater Trochanter Pain Syndrome”. Additionally there may also be pain from the hip joint itself due to wear and tear (osteoarthritis).
Overuse of the gluteal tendons may lead to a situation where the body’s normal tendon repair process becomes overwhelmed and the tendons may become thickened, painful and slightly weakened as a result. This condition may be referred to as tendinopathy or tendinosis rather than the older term tendonitis as there is usually little to no inflammation of the tendon itself.
Tendons may become weaker as part of the normal ageing process. This is similar to the rotator cuff tendons around the shoulder as well as the Achilles tendon in the ankle. As a result, gluteal tendons most commonly cause pain in those over the age of 40. The tendon fibres may fray and start to pull away from the bone, leading to over-loading of the remaining tendon. Whilst it is possible for all of the tendons to come away, it is usually only the front part that does so. This usually causes pain over the outside of the hip, although discomfort may be felt above or below this. Additionally, there may be pain or difficulty lying on the affected side and there may be a noticeable limp, often worse at the end of the day.

Frequently Asked Questions
How are gluteal tears investigated?
Pain over the outside of the upper thigh bone (femur) may be caused by problems with the gluteal tendons. There are 3 gluteal muscles around the hip – the Gluteus Maximus which forms the buttock is the largest and sits behind the hip joint and femur. The two smaller muscles, Gluteus Medius and Gluteus Minimus lie underneath this and join the side of the pelvic bone (ilium) to the top of the femur. They are attached to the outside of the upper femur (the greater trochanter) by strong tendons and act to lift the leg out to the side, a movement known as abduction. Gluteal tendons are often referred to as “abductor” tendons as a result. During normal walking, these muscles stabilise the hip and keep the pelvis level when the opposite foot comes off the ground. This requires them to transmit large forces, typically 2-3 times body weight and over time this may lead to tendon wear.
Lying over the tendons is a small piece of tissue known as the trochanteric bursa – this contains a small amount of fluid and acts to minimise friction from the tough layer of connective tissue (known as the iliotibial band or ITB) that runs over the outside of the femur, down the outside of the leg all the way to the upper shin bone (tibia). Inflammation of this bursa, or a tight ITB can also cause pain and hence these symptoms may also be described as “Trochanteric Bursitis” or “Greater Trochanter Pain Syndrome”. Additionally there may also be pain from the hip joint itself due to wear and tear (osteoarthritis).
Overuse of the gluteal tendons may lead to a situation where the body’s normal tendon repair process becomes overwhelmed and the tendons may become thickened, painful and slightly weakened as a result. This condition may be referred to as tendinopathy or tendinosis rather than the older term tendonitis as there is usually little to no inflammation of the tendon itself.
Tendons may become weaker as part of the normal ageing process. This is similar to the rotator cuff tendons around the shoulder as well as the Achilles tendon in the ankle. As a result, gluteal tendons most commonly cause pain in those over the age of 40. The tendon fibres may fray and start to pull away from the bone, leading to over-loading of the remaining tendon. Whilst it is possible for all of the tendons to come away, it is usually only the front part that does so. This usually causes pain over the outside of the hip, although discomfort may be felt above or below this. Additionally, there may be pain or difficulty lying on the affected side and there may be a noticeable limp, often worse at the end of the day.
How are gluteal tears treated?
Once a full diagnosis is made, your surgeon will work with you to formulate an appropriate treatment plan.
In younger patients, particularly if this has arisen due to a recent increase in physical activity such as joining a gym or taking up running, treatment may include activity restriction and physiotherapy to allow the tendons to recover back to their normal condition. This may be accompanied by gradual strengthening of the gluteal muscles and stretching of the ITB if appropriate. Some physiotherapists my recommend interventions such as dry needling or shock-wave therapy.
Occasionally, ultrasound-guided injections of local anaesthetic and cortisone may be used to aid with diagnosis or to provide a temporary relief of pain to allow progress with physiotherapy. Cortisone injections do not “heal” a tendon tear and repeated injections may in fact weaken the tendons. Injections of PRP (platelet rich plasma) have also been used in the past but there is limited evidence as to their effect.
Where an appropriate period of physiotherapy has not been successful, surgery may be recommended.
What does a gluteal tendon repair involve?
Surgery is performed by 10-12cm incision over the outside of the affected hip. The abnormal bursa tissue is removed and the gluteal tendons are assessed to determine the extent of the tear – frequently, a significant area of tendon has come away from the bone. The bone surface is prepared with the removal of any abnormal spurs to expose healthy bone. The tendons are then re-attached to the bone by the use of specialised suture tape which is passed through the tendons and secured to plastic screw anchors placed within the bone. Further sutures are used to reinforce the repaired tendon to remaining healthy tendon. In many respects this is similar to a rotator cuff repair of the shoulder. If there is co-existent hip osteoarthritis, a hip replacement may be performed in conjunction with a gluteal repair and if there is a tight ITB this may also be releaxed via a small skin incision just above the knee. The wound is then closed and a sterile dressing is applied. We do not usually recommend a brace after this surgery.
If a direct repair is not possible or if a previous repair has re-torn, an alternative tendon transfer procedure may be undertaken. We do not use artificial tendons such as the LARS graft for any gluteal repair surgery.
How long will I stay in hospital?
Most patients will stay overnight, although occasionally some may stay for 2 nights.
What kind of anaesthetic would I have?
There are various types of anaesthetic techniques used in modern practice and your anaesthetist will discuss which would be recommended in your case. Most patients have a light general anaesthetic and are asleep for their surgery. Different types of pain relief are used in combination after surgery to minimise your discomfort.
What is the recovery period?
You will be mobilising with crutches initially and will need to restrict your weight-bearing for a period of 6 weeks to allow the tendon to repair back to the bone surface. After this, you can go down to 1 crutch for a week or 2 and undertake all of your normal daily home activities with full weight-bearing through the affected leg. To minimise the risk of re-tearing the tendons, we usually avoid gluteal strengthening exercises for another 4 weeks. Usually, there is a good reduction in pain within the first few weeks, although significant limping will take several months to improve. Most patients will have difficulty laying on the affected side for 9-12 months after surgery.
What are the risks of surgery?
All surgical procedures can carry some risk and your surgeon will carefully explain these at the time of your consultation.
Do gluteal tears re-occur?
It is possible to re-tear and this unfortunately is due to the tendon itself being weaker than normal. If a tear is small or does not cause significant pain or limping, it may be left alone but if large or very symptomatic, repeat surgery may be considered.
This page is a brief overview and not designed to be all-inclusive. If you have any further queries, please contact us.